Spring allergies are fueled largely by trees—including ash, birch, cedar, alder elm, cottonwood, oak, mesquite, acacia, and pecan. While most tree pollination dies down in May, grasses take the baton starting in June. If your allergies are picking up, you may be feeling the effects of pollen from grass.

(Pixabay / mohamed_hassan)
Beware, the Grass!
There are thousands of species of grass, but only a few produce pollens that are highly allergenic. These include:
- Bahia
- Bermuda
- Brome
- Johnson
- Kentucky Bluegrass
- Meadow Fescue
- Orchard
- Rye
- Timothy
Now that you’re spending more time indoors, you may be able to avoid some contact with grass pollens, but not all. These microscopic pollens can waft in through any open door or window. Avoidance is a nice idea, but it’s not very feasible. Even limited contact with these pollens is enough to make you miserable.
Grasses typically pollinate through summer and end just in time for ragweed season to take over, but that’s a topic for another blog. Whatever the cause of your allergies, you may have noticed that some of your symptoms are similar to the symptoms of covid-19—and that might be making you very nervous. To help put your mind at ease, we’d like to share some information for discerning what is causing your symptoms.
Allergies and Covid-19: Shared Symptoms
Allergies can cause the following symptoms, which are also symptoms of coronavirus:
- Cough—When your body encounters allergens, it can get confused. Rather than your immune system ignoring these harmless particles, it may mistake them for germs and marshal its defenses against them. This involves creating mucus to try to clear these foreign particles out, which can lead to a cough.
- Shortness of breath—The immune system’s response to allergens is to release chemicals into the body that cause inflammation of the airways. This leaves less room for breath to pass through. As a result, people may experience asthma symptoms, including wheezing and shortness of breath.
- Fatigue—Many allergy sufferers complain of fatigue. Sometimes, this is because their allergy symptoms are keeping them from sleeping well at night. Others believe that allergic fatigue results from the body feeling worn down because the immune system is in overdrive trying to “fight off” allergens.
- Sore throat—When chemicals are released during an allergy attack, they can cause the throat to become inflamed. The chemicals also ramp up mucus production that can lead to post-nasal drip (mucus accumulating in the back of the nose and dripping down the back of the throat).
These are the main symptoms that allergies and covid-19 share. The most common allergy symptoms—a runny nose, sneezing and itchy eyes—are not generally associated with covid-19.
How can I Tell the Difference?
So what should you do if you’re experiencing the shared symptoms listed above? Consider these factors that can help you discern between covid-19 and allergies:
- Responsiveness to usual medications. If you’ve experienced cough and shortness of breath before due to allergies, you can take your usual medication and see how your body responds. If you notice that your symptoms don’t improve in the usual way after taking these meds, consult a health care professional.
- Fever. Fever rarely accompanies allergies, so if you are running a high temperature, there is probably something else going on besides seasonal allergies.
- Stomach distress and muscle aches. As with fever, these symptoms are common to novel coronavirus but are not generally associated with pollen allergies.
- Other allergy symptoms. Is your cough/shortness of breath accompanied by other allergy symptoms, such as a runny or stuffed-up nose or itchy eyes? This could be an indicator that your respiratory difficulties are part of a systemic allergic reaction.
- Duration. Allergies are chronic and present with symptoms that may flare up for weeks, months, or years. Covid-19 symptoms tend to come on suddenly.
- Environmental-dependence. Covid-19 symptoms affect you regardless of where you are or the time of day. Allergies are different. You may notice that they are worse when you go outside or at certain times of day when pollen counts are high.
- Severity. Symptoms that are worse than you typically experience with allergies may be an indicator that you are suffering from something different.
Covid-19 Symptoms
As you stay vigilant in watching for signs of covid-19, let’s do a quick recap of symptoms:
- Fever/chills
- Cough
- Shortness of breath
- Muscle pain
- Headache
- Sore throat
- New loss of taste or smell
Though the information we have shared above does not replace personalized guidance from your provider, it can give you a basic idea of what may be going on with your body. Remember, though, that the stakes are high with covid-19, so if in doubt, it’s always best to consult a health care professional.
Could it be Flu or a Cold?
Just as covid-19 can manifest similar to allergies, it can also share symptoms with cold and flu. Here’s a handy chart from Medical News Today to help you know the difference between covid-19 and these other illnesses.
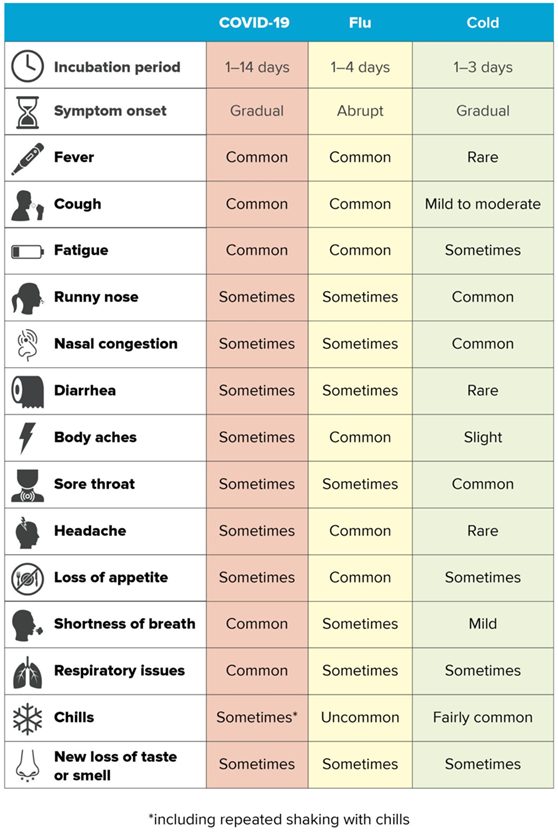
(Image credit: Medical News Today)
How do I Shake These Allergies for Good?
Though it seems hard to believe, once a vaccine is developed, covid-19 won’t dominate virtually every news headline anymore and keep us locked in our homes. Allergies, however, will go on until you get treatment. Medications are helpful in suppressing symptoms, but immunotherapy has been shown to be the only treatment capable of altering the allergic disease itself.
Immunotherapy gets to the heart of the problem—the immune system—desensitizing it to common allergens so that it stops overreacting to them. It is available through allergy shots (subcutaneous immunotherapy) or under-the-tongue allergy drops (sublingual immunotherapy). Both of these treatments are effective for pollen, dust, mold and pet dander allergies. Additionally, allergy drops have been shown to be effective for milk, wheat, and nut allergy treatment.
Stay safe during covid-19. Like you, we’re looking forward to an effective vaccine and treatment for covid-19 and a return to normal life. In the meantime, talk to us about telemedicine options for allergy treatment.


